Published: January 2026 | Medical Review: This guide has been compiled using the latest clinical information from urology and oncology sources.
Bladder cancer is the 6th most common cancer in the United States, with about 81,000 new cases diagnosed annually. This comprehensive guide breaks down everything you need to know—from early warning signs and types to modern treatment options and prevention strategies—helping patients and families navigate diagnosis and beyond with greater clarity.
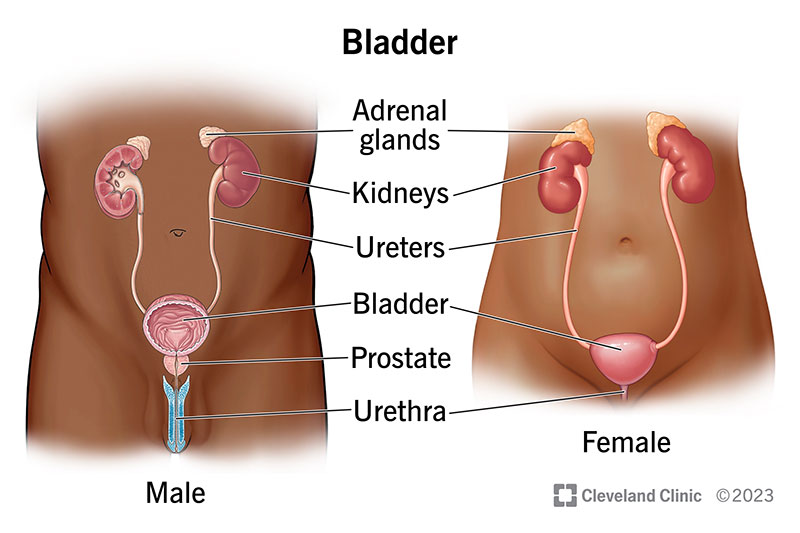
Anatomy of the human bladder (Source: Cleveland Clinic)

Overview infographic of bladder cancer (symptoms, types, and more)
Understanding Bladder Cancer: The Basics
Bladder cancer is the uncontrolled growth of abnormal cells in the urothelium, the lining of the bladder. The bladder is a hollow, muscular organ in the pelvis that stores urine. Most bladder cancers (about 90%) are urothelial carcinomas (also called transitional cell carcinomas), which start in the urothelial cells lining the bladder's interior.
Key Statistics at a Glance
- Annual New Cases (U.S.): ~81,000
- Annual Deaths (U.S.): ~17,000
- Gender Disparity: 3-4 times more common in men (Lifetime risk: 1 in 27 for men, 1 in 89 for women)
- Average Age at Diagnosis: 73 years
- #1 Preventable Risk Factor: Smoking (triples the risk)
Recognizing the Symptoms and Early Signs
Early symptoms can be mistaken for less serious conditions like a urinary tract infection (UTI). Knowing the signs leads to earlier diagnosis and significantly better outcomes.
The most common and often first symptom is hematuria, or blood in the urine. It may be:
- Gross hematuria: Visible, making urine appear pink, red, or cola-colored.
- Microscopic hematuria: Only detectable under a microscope during a urinalysis.
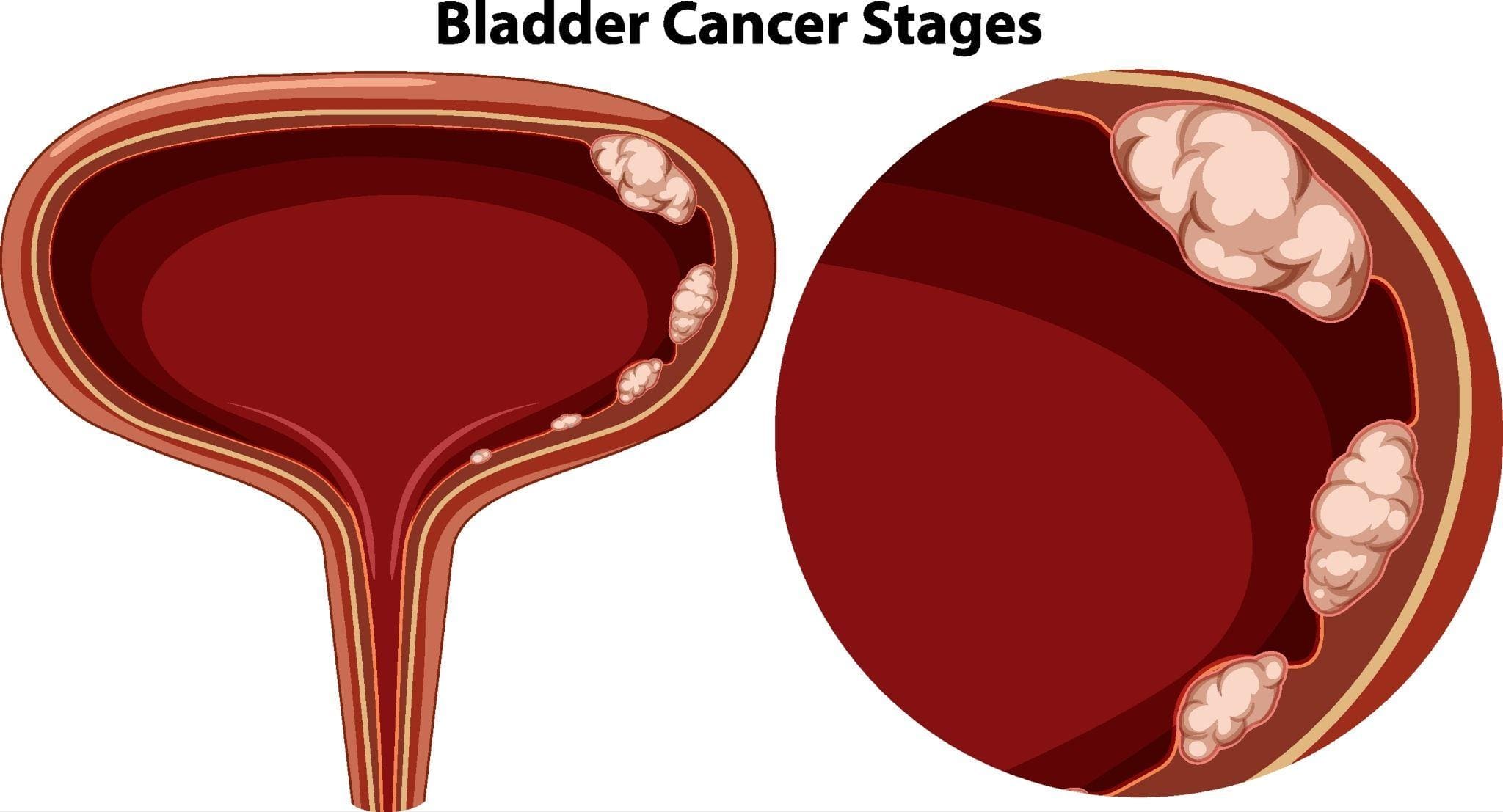
Illustration showing blood in urine (hematuria), a key symptom of bladder cancer
Other symptoms can include:
- Frequent urination
- Pain or a burning sensation during urination (dysuria)
- Feeling an urgent need to urinate
- Feeling the need to urinate without results
- Pelvic or back pain
What Causes Bladder Cancer? Key Risk Factors
Understanding risk factors aids in prevention and proactive health monitoring.

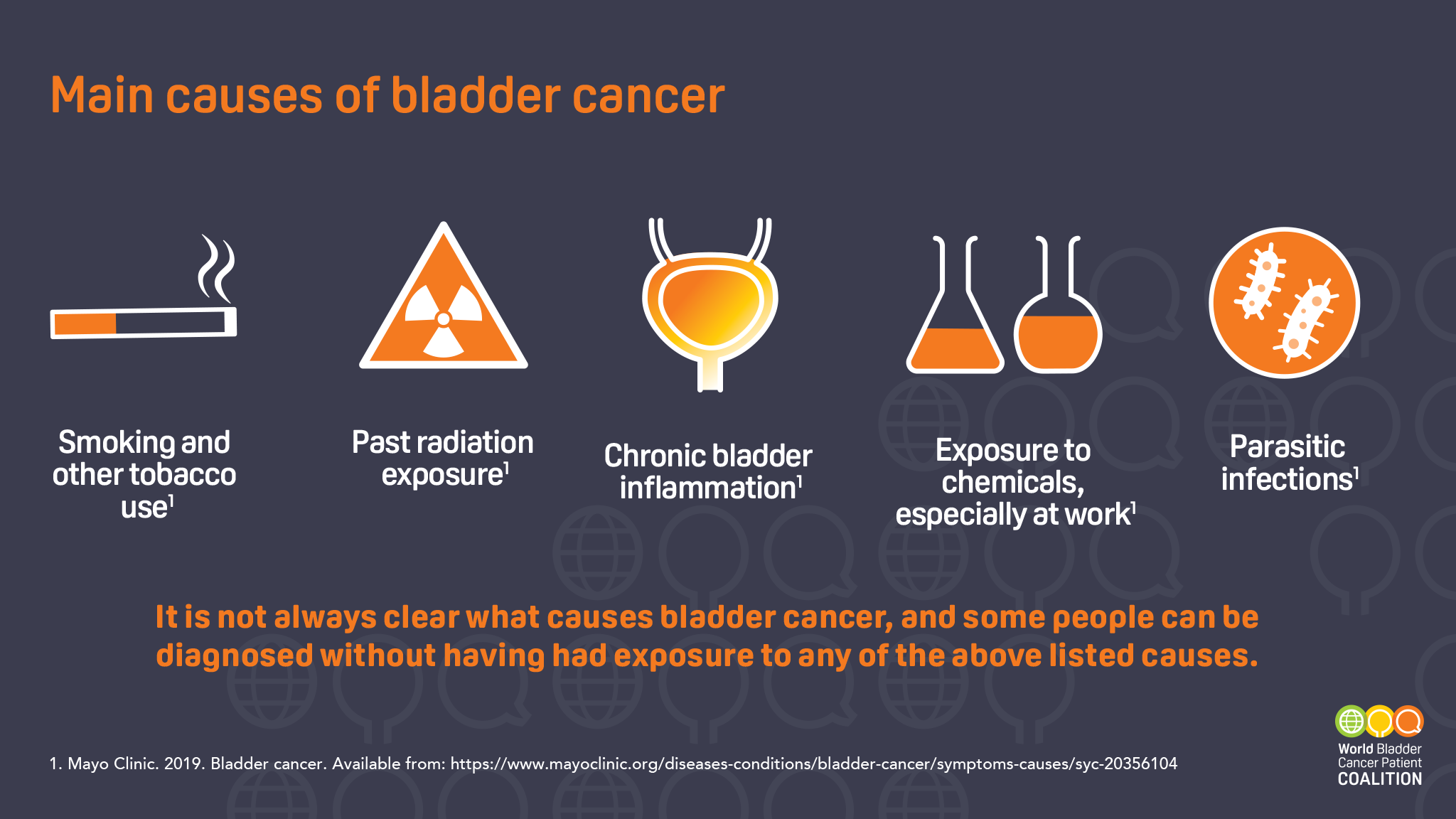
Infographic of key bladder cancer risk factors, including smoking and chemical exposure
Primary Risk Factors Include:
- Smoking: The single greatest preventable risk. Harmful chemicals are filtered by the kidneys and concentrate in urine, damaging bladder lining.
- Chemical Exposure: Occupational exposure to aromatic amines (used in dye, rubber, paint industries).
- Age & Gender: Risk increases with age; men are disproportionately affected.
- Chronic Bladder Irritation: From long-term catheter use or recurrent infections.
- Personal/Family History: Previous bladder cancer or family history of Lynch syndrome.
- Prior Radiation Therapy: Especially to the pelvic region.
Types and Staging: From NMIBC to MIBC
Accurate classification is vital as it dictates treatment.
Main Types of Bladder Cancer
| Type | Description | Prevalence |
|---|---|---|
| Urothelial Carcinoma | Begins in urothelial cells lining the bladder. | ~90% |
| Squamous Cell Carcinoma | Associated with chronic bladder irritation/infection. | 1-2% (U.S.) |
| Adenocarcinoma | Develops from glandular cells; very rare. | <1% |
| Small Cell Carcinoma | Rare, aggressive neuroendocrine tumor. | <1% |
The Critical Distinction: NMIBC vs. MIBC
The most important determination is whether cancer has invaded the muscle layer of the bladder wall.
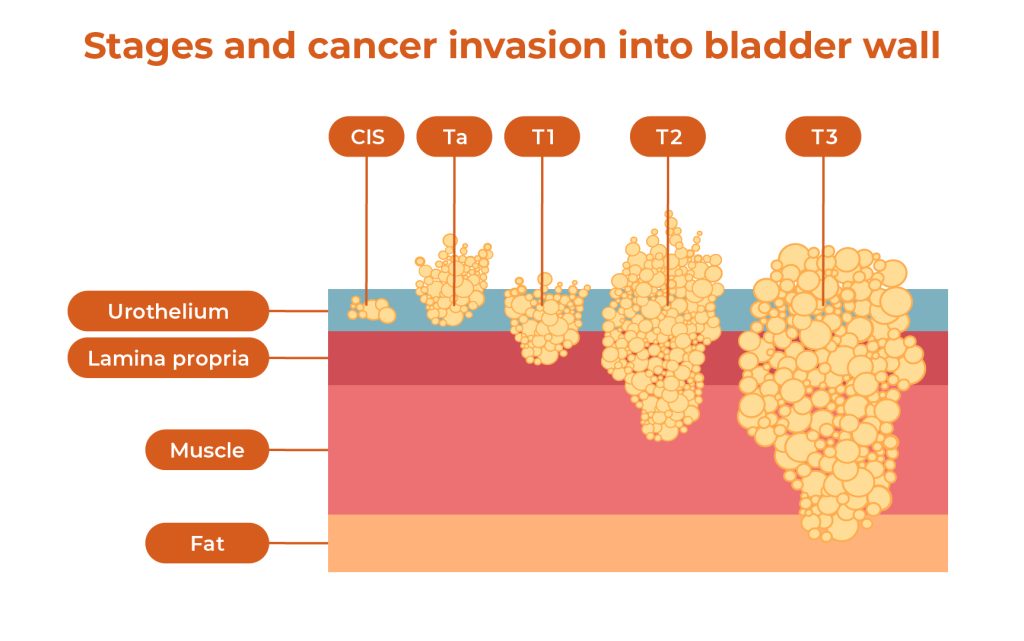
Diagram illustrating non-muscle-invasive vs. muscle-invasive bladder cancer stages
| Feature | Non-Muscle-Invasive (NMIBC) | Muscle-Invasive (MIBC) |
|---|---|---|
| Prevalence at Diagnosis | ~75% of cases | ~25% of cases |
| Depth of Invasion | Inner lining (mucosa) or connective tissue only. | Invades the muscle layer. |
| Metastasis Risk | Low | High |
| Primary Treatment | TURBT + Intravesical Therapy (e.g., BCG) | Radical cystectomy or trimodal therapy |
| 5-Year Survival | Over 90% for Stage 0 | ~70% for localized MIBC |
📊 For a complete visual breakdown of what each stage means, see our detailed guide on Bladder Cancer Stages.
The Diagnosis Process: Step-by-Step
Diagnosis typically follows a structured pathway:

Illustration of cystoscopy, a key diagnostic procedure for bladder cancer
- Initial Evaluation & Urine Tests: Includes medical history, physical exam, urinalysis, and urine cytology to look for cancer cells.
- Cystoscopy: The cornerstone procedure. A urologist inserts a thin, lighted tube (cystoscope) through the urethra to view the bladder lining directly and biopsy any suspicious areas.
- Imaging: A CT urogram or MRI is used to check the upper urinary tracts (kidneys, ureters) and see if cancer has spread.
- TURBT (Transurethral Resection of Bladder Tumor): This is both the definitive diagnostic and initial treatment procedure for NMIBC. The tumor is removed and analyzed to determine its type, grade, and precise stage.
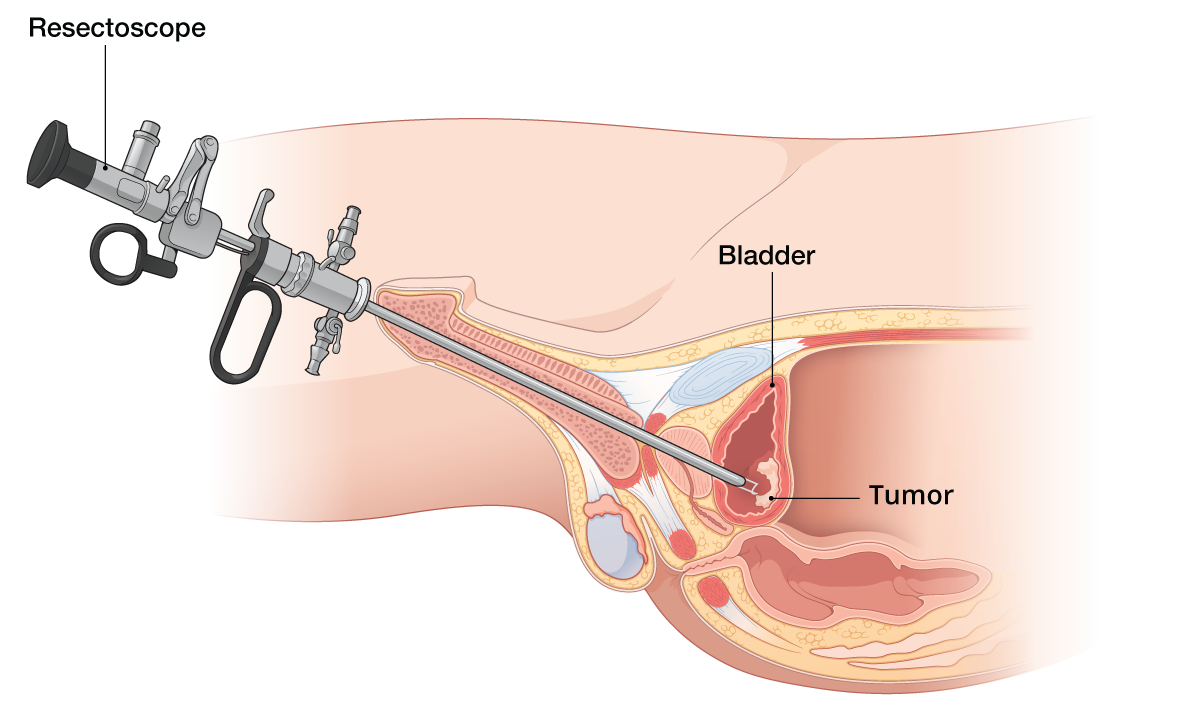
Diagram of Transurethral Resection of Bladder Tumor (TURBT)
Treatment Options by Stage
Treatment is highly personalized based on stage, grade, and overall health.
For Non-Muscle-Invasive Bladder Cancer (NMIBC)
- TURBT: The initial surgical removal of the tumor.
- Intravesical Therapy: Medication delivered directly into the bladder via a catheter to kill remaining cells and prevent recurrence.
- Immunotherapy (BCG): A weakened bacteria that stimulates an immune response against cancer cells. It's the most effective treatment for high-risk NMIBC.
- Chemotherapy: Drugs like mitomycin C or gemcitabine are used to kill cancer cells.
:max_bytes(150000):strip_icc()/bcg-immunotherapy-4843201-ADD-FINAL-V32-7ca128db117246f3a41ebb41acc9abf7.png)
Illustration of BCG immunotherapy delivery into the bladder
Comparing Common Intravesical Therapies:
| Aspect | BCG Immunotherapy | Intravesical Chemotherapy |
|---|---|---|
| Primary Use | High-risk NMIBC, carcinoma in situ (CIS) | Intermediate-risk NMIBC, after TURBT |
| How it Works | Stimulates the body's immune system | Directly kills cancer cells |
| Common Side Effects | Flu-like symptoms, bladder irritation, blood in urine | Bladder irritation, urinary frequency |
| Typical Schedule | Weekly for 6 weeks, then maintenance | Often a single dose post-TURBT |
For Muscle-Invasive Bladder Cancer (MIBC)
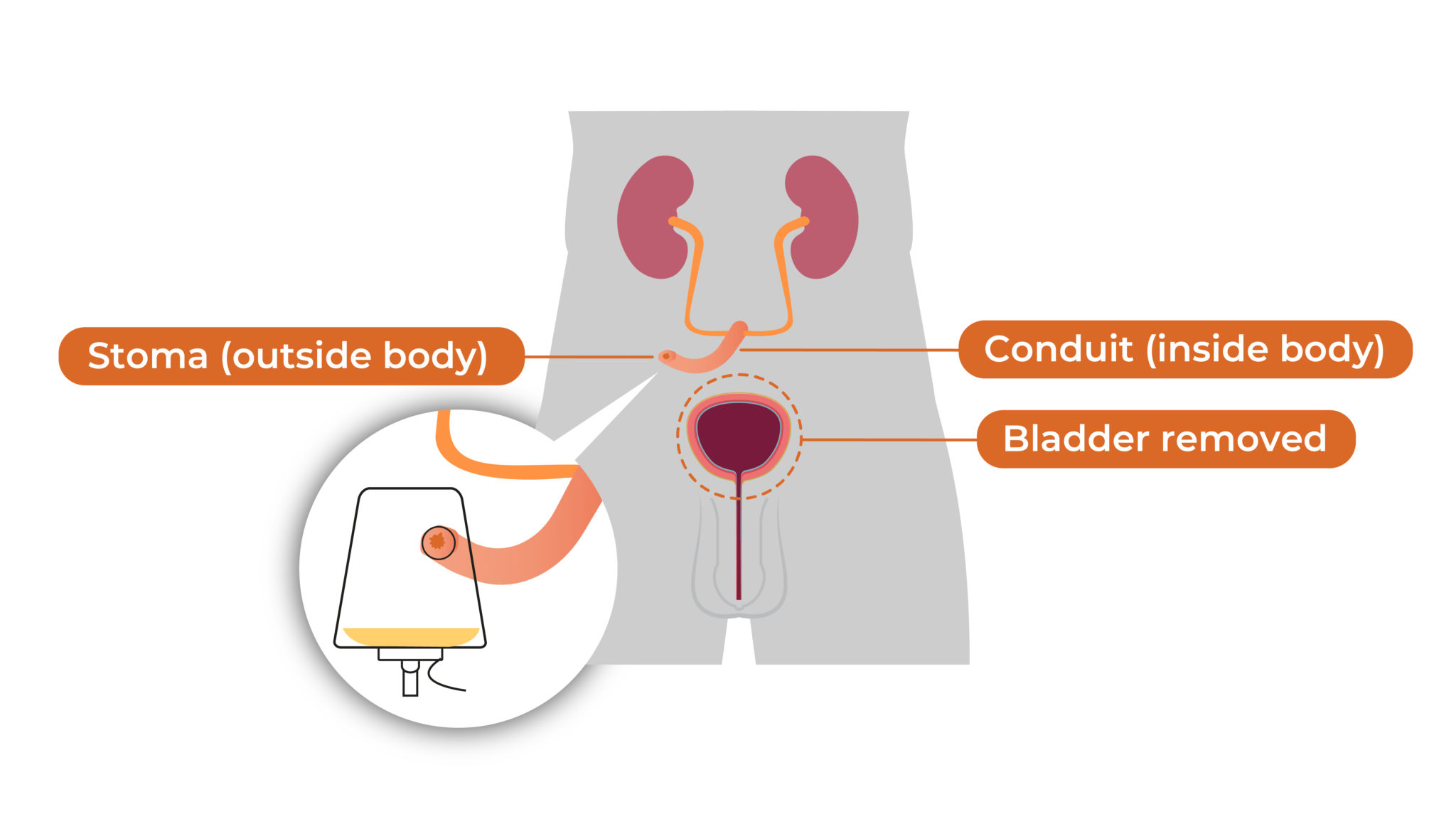
Diagram of radical cystectomy with urinary diversion
- Radical Cystectomy: Surgical removal of the entire bladder and nearby lymph nodes. For men, the prostate may be removed; for women, the uterus and ovaries. Urinary diversion is created.
- Trimodal Therapy (Bladder Preservation): An alternative for select patients, combining a maximal TURBT, radiation therapy, and chemotherapy.
- Chemotherapy: Often given neoadjuvantly (before surgery) to shrink tumors or adjuvantly (after surgery) to target micrometastases.
- Immunotherapy & Targeted Therapy: Used for advanced or metastatic disease (e.g., checkpoint inhibitors like pembrolizumab).
Life After Diagnosis: Survival Rates and Follow-Up
Prognosis varies greatly by stage at diagnosis.

Infographic showing bladder cancer survival rates by stage
5-Year Relative Survival Rates (SEER Data):
- Localized (confined to bladder): 96%
- Regional (spread to nearby tissues/lymph nodes): 47%
- Distant (metastasized): 8%
Life After Treatment: The Follow-Up Schedule
Consistent monitoring is crucial, especially for NMIBC with high recurrence rates. A typical schedule may include:
- First 2 Years: Cystoscopy and urine cytology every 3-6 months.
- Years 3-5: Exams every 6-12 months.
- Beyond 5 Years: Annual monitoring for some patients.
Prevention and Risk Reduction Strategies
Prevention strategies for reducing bladder cancer risk
While not all cases are preventable, you can significantly reduce risk:
- Do Not Smoke: This is the most effective action.
- Limit Chemical Exposure: Follow workplace safety protocols if working with carcinogens.
- Stay Hydrated: Drinking plenty of fluids may dilute potential carcinogens in urine.
- Eat a Balanced Diet: Focus on fruits and vegetables; some evidence suggests a healthy diet may be protective.
Frequently Asked Questions (FAQ)
What is the first sign of bladder cancer?
The most common first sign is painless blood in the urine (hematuria), which may come and go. Even a single episode warrants medical evaluation.
Is bladder cancer curable?
Yes, especially when caught early. The 5-year survival rate for localized, non-muscle-invasive bladder cancer is over 90%. Even muscle-invasive disease can often be cured with aggressive treatment.
What are the newest treatments for bladder cancer?
The field is advancing rapidly. Immunotherapy drugs (checkpoint inhibitors) like pembrolizumab and avelumab are now standard for certain advanced cases. Targeted therapies and antibody-drug conjugates (e.g., enfortumab vedotin) are also showing promise for metastatic disease.
How often does bladder cancer come back?
Recurrence is common with NMIBC, with rates ranging from 30-80% depending on risk factors. This is why long-term, rigorous follow-up with cystoscopy is a standard part of care.
Disclaimer: This guide is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional, such as a urologist or oncologist, for diagnosis, treatment decisions, and personalized medical care.
Comments
Post a Comment